Takotsubo cardiomyopathy
Takotsubo cardiomyopathy, Stress Cardiomyopathy, Broken Heart Syndrome
| Topic | Details |
|---|---|
| 1. Definition |
Takotsubo cardiomyopathy is a transient, reversible form of acute heart failure characterized by sudden weakening of the left ventricular myocardium, typically involving apical ballooning with basal hyperkinesis. It mimics acute coronary syndrome (ACS) but occurs without significant obstructive coronary artery disease. |
| 2. Epidemiology |
Accounts for ~1–2% of all suspected ACS cases. Predominantly affects postmenopausal women (80–90%). Mean age: 60–75 years. Often precipitated by intense emotional or physical stress. |
| 3. Pathophysiology |
Proposed mechanisms include: – Catecholamine surge → myocardial stunning (most accepted). – Microvascular dysfunction. – Coronary artery spasm. – Direct catecholamine toxicity on cardiomyocytes. – Neurogenic stunning via sympathetic overactivation. |
| 4. Triggers |
Emotional: grief, anger, fear, extreme happiness (“happy heart syndrome”). Physical: surgery, sepsis, stroke, asthma attack, acute illness. Idiopathic: no clear trigger in ~30%. |
| 5. Clinical Presentation |
Chest pain (most common, >70%) Dyspnea Syncope (less common) Rarely, cardiogenic shock or sudden cardiac arrest |
| 6. ECG Findings |
ST-segment elevation (often precordial leads, mimicking anterior MI) ST depression, T-wave inversion, QT prolongation possible Absence of ECG changes typical for single coronary territory |
| 7. Biomarkers |
Troponin: mildly elevated (lower than in STEMI relative to wall-motion abnormality) BNP/NT-proBNP: markedly elevated CRP: sometimes elevated in stress states |
| 8. Imaging |
Echocardiography: LV apical ballooning with basal hyperkinesis; possible mid-ventricular, basal, or focal variants. Coronary angiography: normal or non-obstructive coronary arteries. Cardiac MRI: shows myocardial edema without late gadolinium enhancement (helps differentiate from myocarditis or infarction). |
| 9. InterTAK Diagnostic Criteria (Simplified) |
– Transient LV wall motion abnormality extending beyond one coronary territory. – No obstructive coronary disease or acute plaque rupture. – New ECG changes or modest troponin rise. – Absence of myocarditis or pheochromocytoma. |
| 10. Variants |
Classic apical ballooning (most common) Mid-ventricular Basal (inverse Takotsubo) Focal |
| 11. Complications |
Acute heart failure LV outflow tract obstruction (LVOTO) Mitral regurgitation Ventricular arrhythmias LV thrombus and embolic events Rarely, ventricular rupture |
| 12. Management |
– Treat as ACS until diagnosis confirmed. – Acute phase: Oxygen, nitrates, antiplatelets, anticoagulation (initially). – Beta-blockers (reduce catecholamine effect). – ACE inhibitors/ARBs for LV dysfunction. – Diuretics if pulmonary congestion. – Avoid inotropes if LVOTO present. – Anticoagulation for LV thrombus prevention if EF < 30% or thrombus present. – Careful BP and hemodynamic support; mechanical support (IABP, ECMO) if refractory shock. |
| 13. Prognosis |
Generally favorable: full recovery in 1–4 weeks for most patients. Recurrence: 5–10% Mortality: ~4–5% during acute episode (often due to complications) |
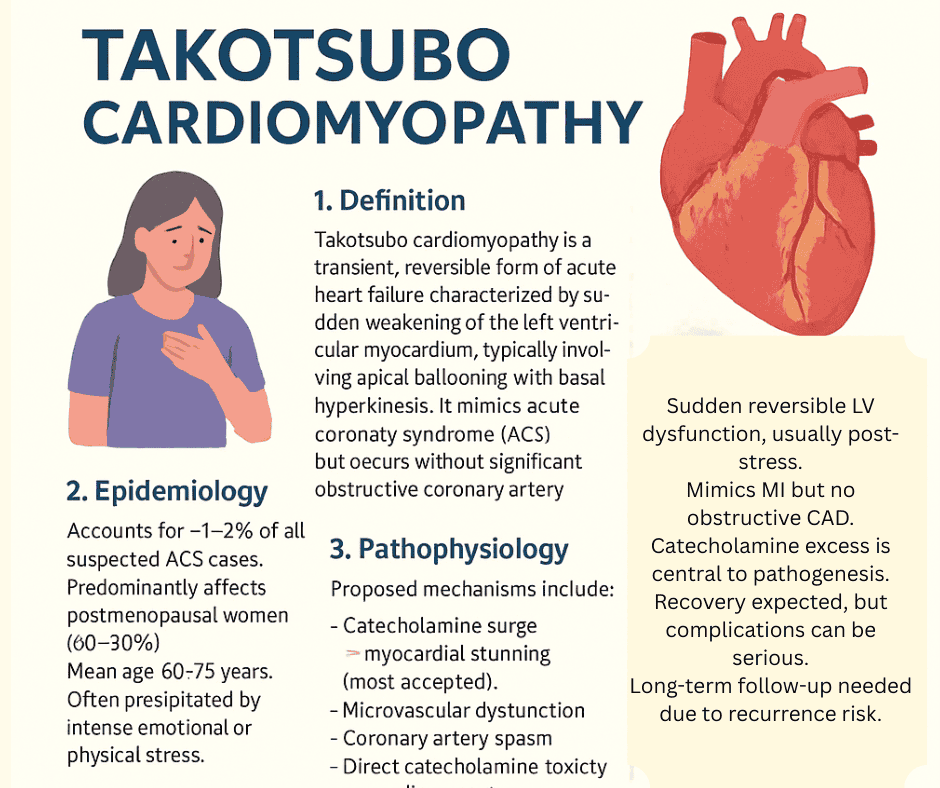
1. Definition
Takotsubo cardiomyopathy is a transient, reversible form of acute heart failure characterized by sudden weakening of the left ventricular myocardium, typically involving apical ballooning with basal hyperkinesis.
It mimics acute coronary syndrome (ACS) but occurs without significant obstructive coronary artery disease.
2. Epidemiology
- Accounts for ~1–2% of all suspected ACS cases.
- Predominantly affects postmenopausal women (80–90%).
- Mean age: 60–75 years.
- Often precipitated by intense emotional or physical stress.
3. Pathophysiology
The exact cause is not fully understood, but proposed mechanisms include:
- Catecholamine surge → myocardial stunning (most accepted).
- Microvascular dysfunction.
- Coronary artery spasm.
- Direct catecholamine toxicity on cardiomyocytes.
- Neurogenic stunning via sympathetic overactivation.
4. Triggers
Emotional: grief, anger, fear, extreme happiness (“happy heart syndrome”).
Physical: surgery, sepsis, stroke, asthma attack, acute illness.
Idiopathic: no clear trigger in ~30%.
5. Clinical Presentation
- Chest pain (most common, >70%)
- Dyspnea
- Syncope (less common)
- Rarely, cardiogenic shock or sudden cardiac arrest
6. ECG Findings
- ST-segment elevation (often precordial leads, mimicking anterior MI)
- ST depression, T-wave inversion, QT prolongation possible
- Absence of ECG changes typical for single coronary territory
7. Biomarkers
- Troponin: mildly elevated (lower than in STEMI relative to wall-motion abnormality)
- BNP/NT-proBNP: markedly elevated
- CRP: sometimes elevated in stress states
8. Imaging
- Echocardiography: LV apical ballooning with basal hyperkinesis; possible mid-ventricular, basal, or focal variants.
- Coronary angiography: normal or non-obstructive coronary arteries.
- Cardiac MRI: shows myocardial edema without late gadolinium enhancement (helps differentiate from myocarditis or infarction).
9. InterTAK Diagnostic Criteria (Simplified)
- Transient LV wall motion abnormality extending beyond one coronary territory.
- No obstructive coronary disease or acute plaque rupture.
- New ECG changes or modest troponin rise.
- Absence of myocarditis or pheochromocytoma.
10. Variants
- Classic apical ballooning (most common)
- Mid-ventricular
- Basal (inverse Takotsubo)
- Focal
11. Complications
- Acute heart failure
- LV outflow tract obstruction (LVOTO)
- Mitral regurgitation
- Ventricular arrhythmias
- LV thrombus and embolic events
- Rarely, ventricular rupture
12. Management
Since presentation mimics ACS, treat as ACS until diagnosis confirmed.
Acute phase:
- Oxygen, nitrates, antiplatelets, anticoagulation (initially)
- Beta-blockers (reduce catecholamine effect)
- ACE inhibitors/ARBs for LV dysfunction
- Diuretics if pulmonary congestion
- Avoid inotropes if LVOTO present (can worsen obstruction)
Specific points:
- Anticoagulation for LV thrombus prevention if EF < 30% or thrombus present.
- Careful BP and hemodynamic support; mechanical support (IABP, ECMO) if refractory shock.
13. Prognosis
- Generally favorable: full recovery in 1–4 weeks for most patients.
- Recurrence: 5–10%
- Mortality: ~4–5% during acute episode (often due to complications)
Key Takeaways
- Sudden reversible LV dysfunction, usually post-stress.
- Mimics MI but no obstructive CAD.
- Catecholamine excess is central to pathogenesis.
- Recovery expected, but complications can be serious.
- Long-term follow-up needed due to recurrence risk.
| Question | Answer |
|---|---|
| 1. What triggers Takotsubo Cardiomyopathy? | Sudden emotional or physical stress causing catecholamine surge. |
| 2. Which heart region shows ballooning in Takotsubo? | The left ventricular apex. |
| 3. What is the typical ECG finding? | ST elevation in anterior precordial leads without coronary blockage. |
| 4. How is Takotsubo diagnosed? | Echocardiography showing apical ballooning plus normal coronary angiography. |
| 5. Who is most affected by Takotsubo? | Postmenopausal women predominantly. |
| 6. What biomarker is mildly elevated? | Troponin. |
| 7. Is the myocardial dysfunction permanent? | No, it is usually reversible within weeks to months. |
| 8. What hormone is implicated in pathophysiology? | Catecholamines (stress hormones). |
| 9. What is the treatment approach? | Supportive care and beta-blockers to reduce stress effects. |
| 10. How to differentiate Takotsubo from MI? | Absence of coronary artery obstruction on angiography. |
| 11. What is the typical prognosis? | Full recovery of heart function within weeks to months. |
| 12. Which imaging shows apical ballooning? | Echocardiography and ventriculography. |
| 13. What gender is predominantly affected? | Females, especially postmenopausal. |
| 14. What is the pathognomonic ventriculogram finding? | Apical ballooning with basal hyperkinesis. |
| 15. Which ECG abnormality mimics acute MI? | ST segment elevation and T wave inversion. |
| 16. What lab marker helps exclude myocarditis? | Cardiac MRI can exclude myocarditis by showing lack of inflammation. |
| 17. What variant involves basal hypokinesis? | Reverse Takotsubo Cardiomyopathy. |
| 18. Can Takotsubo cause cardiogenic shock? | Yes, rarely in severe cases due to LV dysfunction. |
| 19. What is the role of coronary angiography? | To exclude obstructive coronary artery disease. |
| 20. Is thrombolysis indicated in Takotsubo? | No, because it is not caused by coronary thrombosis. |
| 21. What stress hormone surge causes myocardial stunning? | Excess catecholamines like adrenaline and noradrenaline. |
| 22. Are arrhythmias common complications? | They can occur but are not very common. |
| 23. What is the recurrence rate? | Approximately 10% of cases may recur. |
| 24. How long does LV dysfunction last? | Usually resolves within 4–8 weeks. |
| 25. Can beta-blockers prevent recurrence? | Possibly, by mitigating catecholamine effects, but evidence is limited. |
| 26. What symptoms present most commonly? | Chest pain and dyspnea mimicking acute coronary syndrome. |
| 27. Is there permanent scarring of myocardium? | No, myocardial injury is usually reversible without fibrosis. |
| 28. Which population is rarely affected? | Young men and children. |
| 29. Can emotional stress cause other cardiac conditions? | Yes, including arrhythmias and myocardial infarction. |
| 30. What follow-up is recommended? | Repeat echocardiography to monitor recovery of LV function. |


