Stent thrombosis
Stent thrombosis
1. Which of the following is the most common cause of stent thrombosis?
💬 Discontinuation of dual antiplatelet therapy is the leading cause of stent thrombosis, especially early after implantation.
2. Which time frame defines “very late” stent thrombosis?
💬 According to ARC definitions, very late stent thrombosis occurs more than 12 months after stent implantation.
3. What type of stents has a higher incidence of late stent thrombosis?
💬 First-gen DES are more thrombogenic due to delayed endothelialization and polymer issues.
4. Which antiplatelet agent is most associated with stent thrombosis when prematurely stopped?
💬 Premature cessation of clopidogrel is a major cause of stent thrombosis, especially within the first month.
5. Which of the following is a risk factor for early stent thrombosis?
💬 Early thrombosis is often procedural—e.g., underexpansion, dissection, or poor apposition.
6. The diagnosis of stent thrombosis is best confirmed by:
💬 Angiography is the gold standard to visualize thrombus or occlusion in the stented segment.
7. Which condition increases the risk of late stent thrombosis the most?
💬 Diabetes is strongly linked to delayed healing and late stent thrombosis.
8. Optimal DAPT duration for DES to reduce stent thrombosis risk is:
💬 Most guidelines recommend at least 6–12 months of DAPT following DES to reduce thrombosis risk.
9. Which stent feature reduces thrombosis risk in second-generation DES?
💬 Biocompatible or bioabsorbable polymers reduce inflammation and late thrombosis.
10. Stent thrombosis most commonly presents as:
💬 Stent thrombosis often causes abrupt occlusion → STEMI with high mortality.
11. Which imaging modality best assesses stent apposition and expansion?
💬 IVUS provides detailed cross-sectional images to assess stent expansion and apposition, guiding PCI.
12. Stent thrombosis rates are lowest with:
💬 Second-gen DES show reduced stent thrombosis due to better polymers and thinner struts.
13. What is the recommended management for confirmed stent thrombosis?
💬 Urgent PCI is the preferred treatment to restore perfusion in stent thrombosis.
14. The Academic Research Consortium (ARC) classification of stent thrombosis includes:
💬 ARC classifies thrombosis based on certainty: definite, probable, or possible, to standardize studies.
15. Which P2Y12 inhibitor provides the fastest and most potent platelet inhibition?
💬 Prasugrel offers more rapid and potent inhibition of platelet aggregation than clopidogrel.
16. Which of the following increases risk of acute stent thrombosis?
💬 Incomplete stent expansion or malapposition is a key cause of acute thrombosis post-implantation.
17. Very late stent thrombosis is commonly caused by:
💬 Hypersensitivity reactions to stent polymers can cause delayed inflammation and thrombosis.
18. Bioabsorbable scaffolds are associated with:
💬 Early devices had mechanical limitations, causing increased thrombosis risk during resorption.
19. Which laboratory test predicts high platelet reactivity on clopidogrel?
💬 The VerifyNow test assesses P2Y12 receptor inhibition and guides antiplatelet therapy adjustment.
20. Which action best reduces stent thrombosis risk during PCI?
💬 Ensuring full stent expansion with proper apposition is the most important preventive step.
📌 20-Point Summary: Stent Thrombosis
| # | Key Point |
|---|---|
| 1 | Most common cause is premature discontinuation of antiplatelet therapy. |
| 2 | “Very late” stent thrombosis occurs after 1 year post-PCI. |
| 3 | First-generation DES have higher thrombosis risk than second-gen. |
| 4 | Clopidogrel discontinuation is a key factor in early thrombosis. |
| 5 | Procedural issues like underexpansion lead to early thrombosis. |
| 6 | Coronary angiography is the gold standard for diagnosis. |
| 7 | Diabetes is a strong risk factor for late thrombosis. |
| 8 | Recommended DAPT duration after DES is 6–12 months. |
| 9 | Biocompatible polymers in 2nd-gen DES reduce thrombosis. |
| 10 | STEMI is the most common presentation of stent thrombosis. |
| 11 | IVUS helps evaluate stent apposition and expansion. |
| 12 | Second-generation DES have lowest thrombosis rates. |
| 13 | Primary PCI is the treatment of choice for thrombosis. |
| 14 | ARC classifies stent thrombosis as definite, probable, or possible. |
| 15 | Prasugrel provides faster, stronger platelet inhibition. |
| 16 | Underdeployment increases acute thrombosis risk. |
| 17 | Very late thrombosis may result from hypersensitivity to polymers. |
| 18 | Bioabsorbable scaffolds can raise early thrombosis risk. |
| 19 | VerifyNow P2Y12 assay detects high platelet reactivity on clopidogrel. |
| 20 | Ensuring full stent expansion is key to preventing thrombosis. |
📝 Short-Answer Questions (5 Points Each)
-
What is the most common cause of early stent thrombosis?
– Premature discontinuation
– Of dual antiplatelet therapy (DAPT)
– Especially within the first 30 days
– Clopidogrel is often involved
– Emphasizes importance of compliance -
How is “very late” stent thrombosis defined?
– Occurs more than 1 year
– After stent implantation
– Typically due to delayed healing
– Hypersensitivity to polymers
– Or neoatherosclerosis -
List 5 risk factors for stent thrombosis.
– Diabetes mellitus
– Renal failure
– Non-compliance with antiplatelets
– Small vessel diameter
– Bifurcation lesions -
Describe the clinical presentation of stent thrombosis.
– Acute chest pain
– Often mimics STEMI
– Sudden cardiac death possible
– ECG may show ST elevation
– Requires emergency PCI -
Why are second-generation DES preferred over first-generation?
– Lower thrombosis rates
– Improved biocompatibility
– Thinner struts
– Better polymer coatings
– Enhanced endothelialization -
What is the recommended duration of DAPT after DES?
– At least 6–12 months
– Depending on bleeding risk
– Shorter duration for low risk
– Longer for high-risk lesions
– Re-evaluate periodically -
How does intravascular ultrasound (IVUS) help in stent thrombosis?
– Visualizes stent apposition
– Detects under-expansion
– Assesses vessel wall
– Identifies thrombus
– Guides further intervention -
What are the ARC classifications of stent thrombosis?
– Definite
– Probable
– Possible
– Based on timing and evidence
– Used in clinical trials -
Name 5 procedural causes of stent thrombosis.
– Underexpansion
– Malapposition
– Edge dissection
– Incomplete lesion coverage
– Inadequate post-dilation -
How does platelet function testing help in thrombosis prevention?
– Detects resistance to drugs
– Like clopidogrel
– VerifyNow is commonly used
– High reactivity predicts risk
– Helps guide therapy change
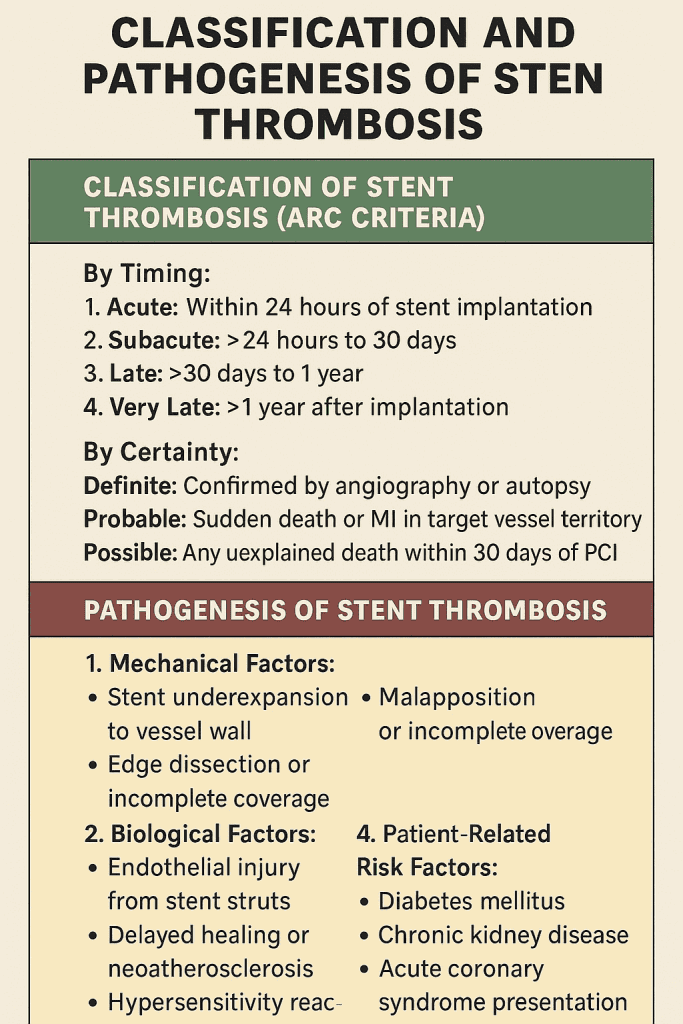
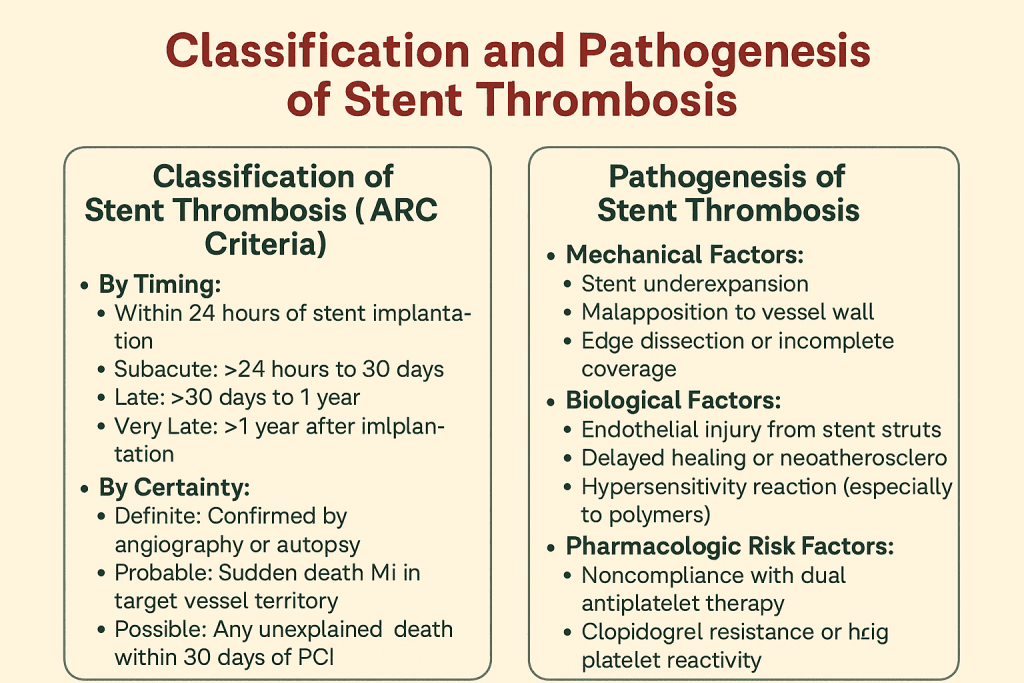
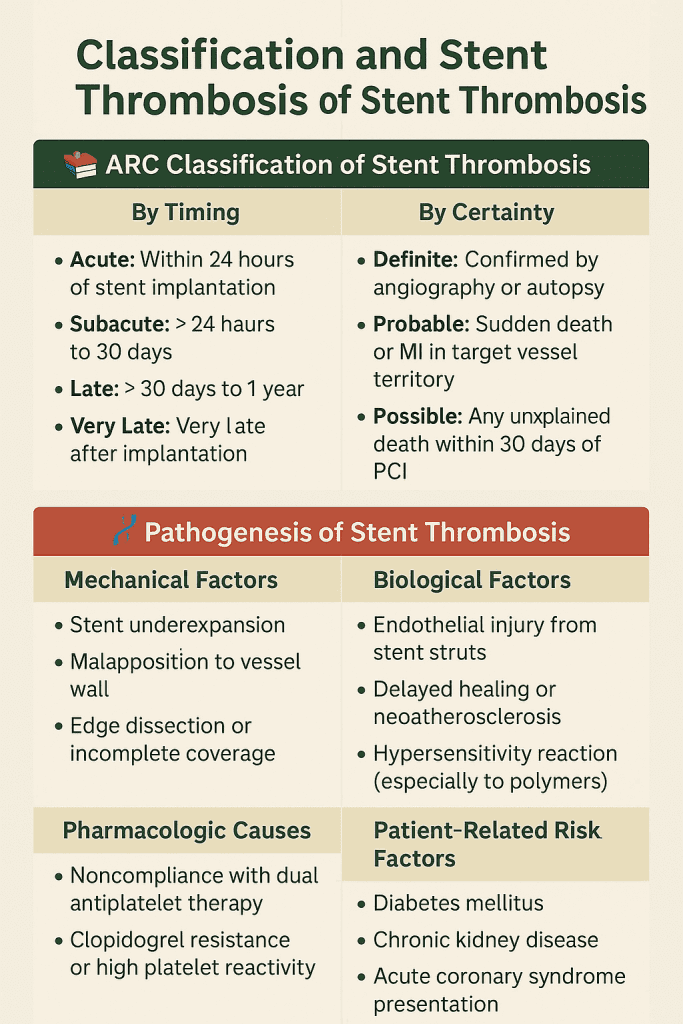
📚 ARC Classification of Stent Thrombosis
- 1. Acute: Within 24 hours of stent implantation
- 2. Subacute: >24 hours to 30 days
- 3. Late: >30 days to 1 year
- 4. Very Late: >1 year after implantation
By Certainty:
- Definite: Confirmed by angiography or autopsy
- Probable: Sudden death or MI in target vessel territory
- Possible: Any unexplained death within 30 days of PCI
🧬 Pathogenesis of Stent Thrombosis
- 1. Mechanical Factors:
- Stent underexpansion
- Malapposition to vessel wall
- Edge dissection or incomplete coverage
- 2. Biological Factors:
- Endothelial injury from stent struts
- Delayed healing or neoatherosclerosis
- Hypersensitivity reaction (especially to polymers)
- 3. Pharmacologic Causes:
- Noncompliance with dual antiplatelet therapy
- Clopidogrel resistance or high platelet reactivity
- 4. Patient-Related Risk Factors:
- Diabetes mellitus
- Chronic kidney disease
- Acute coronary syndrome presentation
| Feature | Stent Thrombosis | Restenosis |
|---|---|---|
| Definition | Formation of thrombus (clot) inside the stent | Re-narrowing of the stented vessel due to neointimal hyperplasia |
| Time of Onset | Early (within days) to late (>1 year) | Typically after weeks to months |
| Clinical Presentation | Acute coronary syndrome, sudden death | Gradual angina recurrence |
| Mechanism | Platelet aggregation, clot formation | Smooth muscle proliferation, extracellular matrix buildup |
| Trigger | Mechanical issues, DAPT noncompliance | Natural healing response, vessel injury |
| Diagnostic Method | Angiography shows thrombus | Angiography shows gradual narrowing |
| Treatment | Urgent PCI, thrombolysis, antiplatelet therapy | Repeat PCI, drug-eluting balloon, re-stenting |
| Prognosis | High mortality if untreated | Better prognosis, more gradual course |
LAD Coronary Artery
LAD Coronary Artery Restart Quiz 🫀 20 High-Yield Facts About the LAD Coronary Artery 1. LAD is a branch of the LMCA + The Left Anterior Descending artery originates from the Left Main Coronary Artery (LMCA). 2. Supplies anterior 2/3 of septum + LAD perfuses the anterior 2/3 of the interventricular septum including bundle branches. 3. Supplies anterior wall of LV + The LAD is responsible for perfusing the anterior wall of the left ventricle. 4. Known as the “Widow-Maker” + A proximal LAD occlusion often causes massive MI or sudden cardiac death. 5. ST elevation in V1–V4 + Anterior...


