Right atrial (RA) pressure
Right atrial (RA) pressure
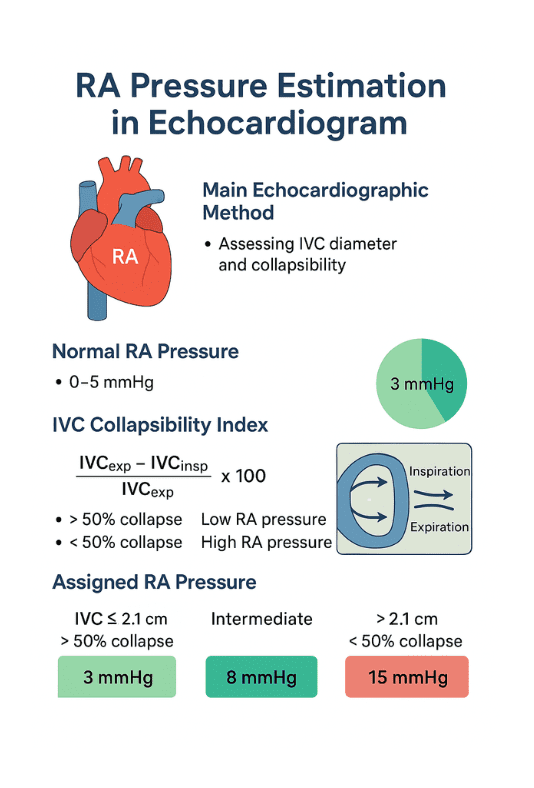
| IVC Diameter | Respiratory Variation | Estimated RA Pressure |
|---|---|---|
| ≤ 2.1 cm | > 50% collapse with inspiration | 3 mmHg (range 0–5 mmHg) |
| > 2.1 cm | < 50% collapse with inspiration | 15 mmHg (range 10–20 mmHg) |
| Intermediate findings | Variable collapse | 8 mmHg (range 5–10 mmHg) |
| Parameter | Criteria | Estimated RA Pressure | Clinical Notes |
|---|---|---|---|
| IVC diameter < 2.1 cm + > 50% collapse with sniff | Normal size, good collapse | 3 mmHg (range 0–5) | Suggests normal RA pressure and normal RAP waveform |
| IVC diameter > 2.1 cm + < 50% collapse | Dilated, poor collapse | 15 mmHg (range 10–20) | Suggests elevated RA pressure; check for RV dysfunction, pulmonary hypertension |
| Mixed pattern | Either small diameter + poor collapse OR large diameter + good collapse | 8 mmHg (range 5–10) | Intermediate category; consider other echo signs (hepatic vein flow, RA size) |
| Markedly dilated IVC, fixed diameter | No inspiratory collapse | 20 mmHg+ | Seen in tamponade, severe TR, constrictive pericarditis |
| IVC < 1.5 cm, collapses fully | Very compliant | 0–3 mmHg | Often seen in hypovolemia |
| Use in TR velocity–Bernoulli calculation | Add estimated RA pressure to RV–RA gradient | — | Essential for RVSP calculation |
| Alternative signs when IVC view not possible | Hepatic vein flow, RA area, right heart strain | Varies | Used when subcostal IVC imaging is suboptimal |
| Respiratory variation considerations | Assess collapse with sniff or quiet inspiration | — | Avoid deep exaggerated inspirations in patients with lung disease |
| No. | Key Point | Details |
|---|---|---|
| 1 | Purpose of RA Pressure Estimation | Helps assess right heart hemodynamics and estimate pulmonary artery systolic pressure (PASP). |
| 2 | Commonly Used Method | Based on Inferior Vena Cava (IVC) diameter and collapsibility with respiration. |
| 3 | Normal IVC Size | ≤ 2.1 cm in diameter. |
| 4 | Normal IVC Collapse | ≥ 50% collapse during a sniff indicates normal RA pressure. |
| 5 | Low RA Pressure | Typically 3 mmHg (range 0–5 mmHg) when IVC is normal in size and collapses > 50%. |
| 6 | Intermediate RA Pressure | Approximately 8 mmHg for intermediate findings. |
| 7 | High RA Pressure | 15 mmHg (range 10–20 mmHg) when IVC is dilated > 2.1 cm and collapses < 50%. |
| 8 | Severe RA Pressure Elevation | May exceed 20 mmHg in severe pulmonary hypertension or right heart failure. |
| 9 | Additional Clues | Hepatic vein flow reversal suggests elevated RA pressure. |
| 10 | Exercise or Stress Echo | RA pressure estimation can change dynamically with stress testing. |
| 11 | 2D vs. M-mode | 2D imaging preferred for accurate IVC measurement; M-mode may overestimate collapsibility. |
| 12 | Subcostal View | Preferred echocardiographic view for IVC assessment. |
| 13 | Technical Pitfalls | Poor subcostal windows, obesity, and mechanical ventilation can affect accuracy. |
| 14 | Effect of Mechanical Ventilation | Positive pressure can reduce IVC collapsibility and falsely elevate estimated RA pressure. |
| 15 | RVSP Calculation Link | RA pressure is added to TR jet gradient for right ventricular systolic pressure (RVSP). |
| 16 | Invasive Correlation | Right heart catheterization is the gold standard for RA pressure measurement. |
| 17 | Role in Heart Failure | Elevated RA pressure indicates systemic venous congestion in right heart failure. |
| 18 | Role in Pulmonary Hypertension | Helps in estimating pulmonary artery pressures and disease severity. |
| 19 | Serial Measurement | Useful for monitoring treatment response in heart failure or pulmonary hypertension. |
| 20 | ASE Guideline Reference | Based on American Society of Echocardiography recommendations for chamber quantification. |
1. What is the main echocardiographic method for estimating RA pressure?
- By assessing inferior vena cava (IVC) diameter and its collapsibility during inspiration.
- Uses subcostal long-axis view.
- IVC ≤ 2.1 cm with > 50% collapse → normal RA pressure (~3 mmHg).
- IVC > 2.1 cm with < 50% collapse → high RA pressure (~15 mmHg).
- Intermediate findings → RA pressure ~8 mmHg.
2. What is the normal RA pressure range in echocardiography?
- Typically 0–5 mmHg in healthy adults.
- ASE guidelines use 3 mmHg for low, 8 mmHg for intermediate, 15 mmHg for high.
- Based on IVC size and collapsibility index.
- Values are estimates, not invasive measurements.
- Catheterization confirms actual pressure.
3. What is IVC collapsibility index?
- Formula: (IVC_exp – IVC_insp) / IVC_exp × 100.
- 50% collapse → low RA pressure.
- < 50% collapse → elevated RA pressure.
- Measured during sniff or deep inspiration.
- Reflects right atrial filling pressure changes.
4. Which factors can falsely elevate RA pressure estimation?
- Mechanical ventilation (positive pressure).
- Athletes with large compliant IVC.
- Severe tricuspid regurgitation.
- Pericardial diseases (tamponade, constriction).
- Increased intra-abdominal pressure.
5. How does mechanical ventilation affect RA pressure estimation?
- Positive pressure reduces IVC collapse.
- Can mimic high RA pressure.
- Inverse relationship with spontaneous breathing findings.
- Requires cautious interpretation.
- In such cases, invasive measurement is more reliable.
6. What RA pressure value is assigned to IVC ≤ 2.1 cm with > 50% collapse?
- 3 mmHg (low RA pressure).
- Suggests normal right-sided filling pressures.
- Often seen in healthy individuals.
- No significant right heart overload.
- Confirms adequate venous return compliance.
7. What RA pressure value is assigned to IVC > 2.1 cm with < 50% collapse?
- 15 mmHg (high RA pressure).
- Suggests right-sided congestion.
- Often seen in heart failure, pulmonary hypertension.
- Indicates elevated venous pressures.
- Requires further clinical correlation.
8. What does an intermediate IVC pattern indicate?
- IVC size and collapsibility do not fit extremes.
- Assigned 8 mmHg RA pressure.
- Reflects moderate right atrial pressure.
- May occur in early right heart dysfunction.
- Interpretation depends on clinical context.
9. How is RA pressure related to pulmonary artery systolic pressure (PASP) estimation?
- PASP = 4 × (TR velocity)² + RA pressure.
- TR velocity measured via Doppler.
- Accurate RA pressure estimation improves PASP accuracy.
- Overestimation can lead to false diagnosis of pulmonary hypertension.
- Underestimation can miss severe cases.
10. Why is invasive measurement sometimes preferred over echo estimation?
- Echocardiography is indirect and assumption-based.
- Invasive right heart catheterization measures RA pressure directly.
- Needed when clinical suspicion is high but echo is inconclusive.
- Useful in complex cardiopulmonary disease.
- Provides gold-standard hemodynamic data.
| Parameter | Criteria | Estimated RA Pressure | Clinical Notes |
|---|---|---|---|
| IVC diameter < 2.1 cm + > 50% collapse with sniff | Normal size, good collapse | 3 mmHg (range 0–5) | Suggests normal RA pressure and normal RAP waveform |
| IVC diameter > 2.1 cm + < 50% collapse | Dilated, poor collapse | 15 mmHg (range 10–20) | Suggests elevated RA pressure; check for RV dysfunction, pulmonary hypertension |
| Mixed pattern | Either small diameter + poor collapse OR large diameter + good collapse | 8 mmHg (range 5–10) | Intermediate category; consider other echo signs (hepatic vein flow, RA size) |
| Markedly dilated IVC, fixed diameter | No inspiratory collapse | 20 mmHg+ | Seen in tamponade, severe TR, constrictive pericarditis |
| IVC < 1.5 cm, collapses fully | Very compliant | 0–3 mmHg | Often seen in hypovolemia |
| Use in TR velocity–Bernoulli calculation | Add estimated RA pressure to RV–RA gradient | — | Essential for RVSP calculation |
| Alternative signs when IVC view not possible | Hepatic vein flow, RA area, right heart strain | Varies | Used when subcostal IVC imaging is suboptimal |
| Respiratory variation considerations | Assess collapse with sniff or quiet inspiration | — | Avoid deep exaggerated inspirations in patients with lung disease |


