Jugular venous pressure
Jugular venous pressure
21. The ‘a’ wave in JVP occurs due to:
A. Closure of tricuspid valve
B. Right atrial contraction
C. Right ventricular systole
D. Atrial filling from IVC
Explanation: The ‘a’ wave in the jugular venous waveform corresponds to atrial contraction just before the tricuspid valve closes.
22. Which JVP component represents tricuspid valve bulging into the right atrium?
A. a wave
B. x descent
C. c wave
D. y descent
Explanation: The ‘c’ wave in the JVP reflects the tricuspid valve bulging into the right atrium during early right ventricular contraction.
23. Which component of JVP is absent in atrial fibrillation?
A. a wave
B. c wave
C. v wave
D. y descent
Explanation: The ‘a’ wave is due to atrial contraction and is absent in atrial fibrillation due to uncoordinated atrial activity.
24. The ‘x’ descent represents:
A. Atrial contraction
B. Atrial relaxation and downward displacement of tricuspid valve
C. Atrial filling
D. Ventricular filling
Explanation: The ‘x’ descent occurs due to atrial relaxation and downward movement of the tricuspid valve during ventricular systole.
25. The prominent ‘v’ wave in JVP is commonly seen in:
A. Tricuspid stenosis
B. Tricuspid regurgitation
C. Constrictive pericarditis
D. Cardiac tamponade
Explanation: Tricuspid regurgitation causes retrograde flow into the right atrium during systole, producing prominent ‘v’ waves.
26. The ‘y’ descent represents:
A. Passive emptying of RA into RV after tricuspid valve opens
B. Ventricular systole
C. Atrial contraction
D. Ventricular filling
Explanation: The ‘y’ descent occurs due to the passive emptying of the right atrium into the right ventricle when the tricuspid valve opens.
27. Which condition shows steep ‘y’ descent?
A. Cardiac tamponade
B. Constrictive pericarditis
C. Tricuspid stenosis
D. Pulmonary hypertension
Explanation: Constrictive pericarditis causes rapid early diastolic filling, resulting in a steep ‘y’ descent in the JVP waveform.
28. Kussmaul’s sign refers to:
A. Disappearance of JVP on inspiration
B. Paradoxical rise in JVP on inspiration
C. Absence of ‘a’ wave
D. Giant ‘v’ wave
Explanation: Kussmaul’s sign is a paradoxical increase in JVP during inspiration, typically seen in constrictive pericarditis and right heart failure.
29. In cardiac tamponade, the JVP shows:
A. Steep x and y descents
B. Prominent x descent with blunted y descent
C. Cannon ‘a’ waves
D. Large ‘v’ wave
Explanation: Cardiac tamponade results in a prominent x descent due to atrial relaxation, but y descent is blunted due to limited ventricular filling.
30. Cannon ‘a’ waves are typically seen in:
A. Atrial fibrillation
B. Complete heart block
C. Sinus bradycardia
D. Tricuspid regurgitation
Explanation: Cannon ‘a’ waves occur when the atria contract against a closed tricuspid valve, commonly seen in complete heart block due to AV dissociation.
Jugular venous pressure
| 1 | JVP reflects right atrial pressure and is a marker of right heart function. |
| 2 | Best assessed via the right internal jugular vein due to its direct connection to the right atrium. |
| 3 | Normal JVP is ≤ 4 cm above the sternal angle (≈ 8–9 cm H2O absolute). |
| 4 | Position patient at 30–45° to visualize the pulsation clearly. |
| 5 | The JVP waveform has a, c, and v waves; and x and y descents. |
| 6 | ‘a’ wave: right atrial contraction – absent in atrial fibrillation. |
| 7 | ‘c’ wave: bulging of tricuspid valve into right atrium during early systole. |
| 8 | ‘v’ wave: passive filling of right atrium against closed tricuspid valve. |
| 9 | ‘x’ descent: atrial relaxation and downward displacement of tricuspid valve. |
| 10 | ‘y’ descent: tricuspid valve opens, passive ventricular filling. |
| 11 | Prominent ‘a’ wave: seen in tricuspid stenosis, pulmonary hypertension. |
| 12 | Cannon ‘a’ waves: complete heart block, AV dissociation. |
| 13 | Prominent ‘v’ wave: tricuspid regurgitation. |
| 14 | Steep ‘y’ descent: constrictive pericarditis. |
| 15 | Absent ‘y’ descent: cardiac tamponade. |
| 16 | Kussmaul’s sign: rise in JVP on inspiration – seen in constrictive pericarditis. |
| 17 | Hepatojugular reflux accentuates JVP by increasing venous return. |
| 18 | Carotid pulse is palpable and has one upstroke; JVP is biphasic and non-palpable. |
| 19 | JVP normally falls with inspiration due to negative intrathoracic pressure. |
| 20 | Elevated JVP is an important sign in heart failure, volume overload, and right heart pathology. |
Mechanism
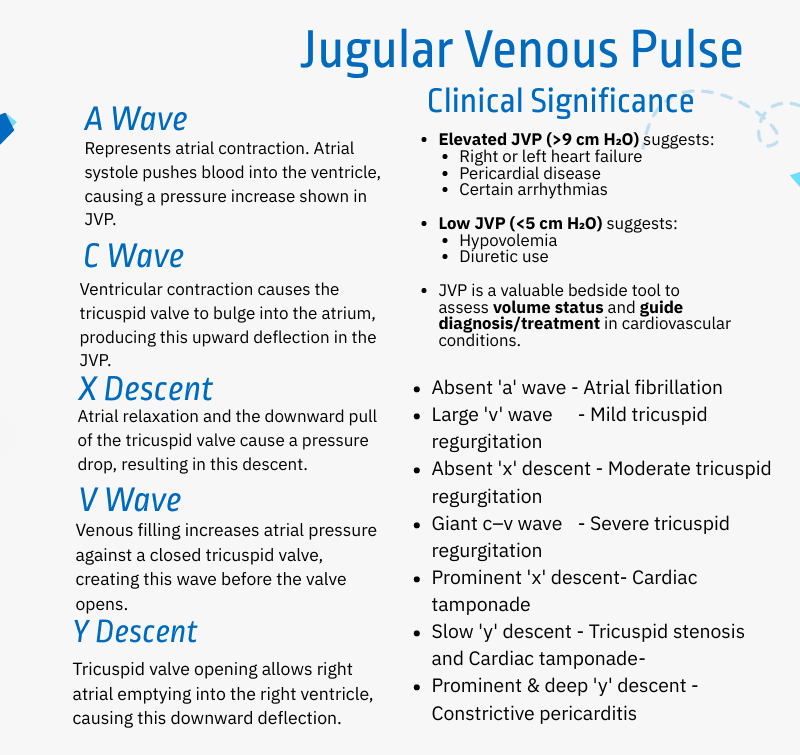
The jugular venous pulse (JVP) waveform is biphasic and includes several peaks and troughs:
- A wave: Atrial contraction (atrial systole)
- C wave: Bulging of the tricuspid valve during right ventricular contraction
- X descent: Atrial relaxation and downward movement of the tricuspid valve
- V wave: Venous filling against a closed tricuspid valve
- Y descent: Opening of the tricuspid valve and emptying of the right atrium into the right ventricle
Pathophysiology
- Atrial fibrillation: Absent A wave and diminished X descent due to lack of atrial contraction.
- Pulmonary or tricuspid stenosis: Enlarged A wave and blunted Y descent from increased resistance.
- AV dissociation (e.g., complete heart block): Simultaneous atrial and ventricular contraction produces Cannon A waves.
- Tricuspid regurgitation: Backflow during systole leads to reduced X descent or formation of a CV wave.
- Cardiac tamponade: Severely reduced or absent Y descent due to pressure from the pericardial sac.
- Constrictive pericarditis: Prominent Y descent (Friedreich’s sign) due to abrupt emptying of the right atrium into a stiff ventricle.
Clinical Significance
- Elevated JVP (>9 cm H₂O): Indicates venous hypertension, often due to heart failure, pericardial disease, or arrhythmias.
- Low JVP (<5 cm H₂O): Suggests hypovolemia or diuretic use.
- JVP analysis aids in evaluating volume status, cardiac function, and guiding treatment decisions in clinical practice.
- Elevated JVP (>9 cm H₂O) suggests:
- Right or left heart failure
- Pericardial disease
- Certain arrhythmias
- Low JVP (<5 cm H₂O) suggests:
- Hypovolemia
- Diuretic use
- JVP is a valuable bedside tool to assess volume status and guide diagnosis/treatment in cardiovascular conditions.
Jugular Venous Pressure (JVP) Waveform – 20 Key Points Table
| No. | Wave/Descent | Description | Physiology | Clinical Significance |
|---|---|---|---|---|
| 1️⃣ | a wave | First upward deflection | Atrial contraction | Absent in atrial fibrillation |
| 2️⃣ | c wave | Small upward notch | Bulging of tricuspid valve during ventricular systole | Often subtle; seen in normal JVP |
| 3️⃣ | x descent | Downward slope after ‘a’ | Atrial relaxation and downward pull of tricuspid valve | Prominent in cardiac tamponade |
| 4️⃣ | v wave | Second upward deflection | Venous filling of right atrium during late systole | Large in tricuspid regurgitation |
| 5️⃣ | y descent | Sharp fall after ‘v’ wave | Passive emptying of atrium into ventricle | Prominent in constrictive pericarditis |
| 6️⃣ | a–c interval | Small rise between ‘a’ and ‘c’ | Ventricular systole begins | Rarely visible separately |
| 7️⃣ | c–x interval | Dip after c wave | Ventricular ejection | Reflects tricuspid valve descent |
| 8️⃣ | v–y interval | Peak then fall | Passive filling then emptying | Altered in right heart failure |
| 9️⃣ | Cannon a wave | Large ‘a’ wave | Atria contract against closed tricuspid valve | Seen in complete heart block, VT |
| 🔟 | Absent a wave | Flat baseline | No atrial contraction | Atrial fibrillation |
| 1️⃣1️⃣ | Giant v wave | Very large v wave | Tricuspid regurgitation | Rapid atrial filling against closed valve |
| 1️⃣2️⃣ | Slow y descent | Blunted drop after v | Impaired RV filling | Seen in tamponade or RV infarct |
| 1️⃣3️⃣ | Rapid y descent | Sharp fall | Unrestricted ventricular filling | Seen in constrictive pericarditis |
| 1️⃣4️⃣ | Steep x descent | Deep drop after c | Efficient atrial relaxation | Seen in tamponade or hypovolemia |
| 1️⃣5️⃣ | Wave fusion | a + v overlap | Tachycardia | Difficult wave identification |
| 1️⃣6️⃣ | Paradoxical JVP rise | Increase with inspiration | Kussmaul’s sign | Seen in constriction, RV failure |
| 1️⃣7️⃣ | Prominent a wave | Tall initial wave | RV hypertrophy, pulmonary HTN | Atrial contraction against stiff RV |
| 1️⃣8️⃣ | Flickering JVP | Rapid oscillations | Hyperdynamic state | Seen in anemia, thyrotoxicosis |
| 1️⃣9️⃣ | JVP height measurement | Vertical from sternal angle | Reflects RA pressure | >3 cm = elevated JVP |
| 2️⃣0️⃣ | JVP waveform vs carotid | Biphasic, collapsible, non-palpable | Differentiates from carotid pulse | Important clinical distinction |
Short questions about Jugular Venous Pressure (JVP) waveforms, each followed by 5 concise -point answers explaining key facts or clinical correlations:
1. What does the ‘a’ wave in the JVP represent?
- Atrial contraction during end-diastole
- Occurs just before the first heart sound (S1)
- Absent in atrial fibrillation
- Prominent in tricuspid stenosis
- Best seen with synchronized ECG (P wave)
2. When is the ‘a’ wave absent in the JVP?
- Atrial fibrillation (no atrial contraction)
- Junctional rhythms without retrograde P waves
- Ventricular pacing
- AV dissociation
- Sinus arrest
3. What causes a giant ‘a’ wave in JVP?
- Tricuspid stenosis
- Pulmonary hypertension
- Right ventricular hypertrophy
- Junctional rhythm with retrograde block
- AV dissociation (e.g., complete heart block)
4. What is the ‘c’ wave in the JVP waveform?
- Bulging of tricuspid valve into right atrium
- Occurs during early systole
- Coincides with isovolumetric contraction
- May be indistinct or merged with other waves
- Small or absent in normal individuals
5. What does the ‘x’ descent represent?
- Atrial relaxation
- Downward pull of tricuspid valve during ventricular systole
- Seen between ‘a’ and ‘v’ waves
- Prominent in cardiac tamponade
- Often steeper than the y-descent
6. What causes a prominent ‘x’ descent?
- Constrictive pericarditis
- Tamponade (when y-descent is blunted)
- Tricuspid regurgitation (if ‘x’ is preserved)
- Dehydration (low-volume states)
- Normal physiology with vigorous right ventricular contraction
7. What does the ‘v’ wave signify?
- Passive venous filling of right atrium
- Occurs during late systole
- Peaks just before tricuspid valve opens
- Prominent in tricuspid regurgitation
- Follows the ‘x’ descent
8. What causes a giant ‘v’ wave?
- Severe tricuspid regurgitation
- Increased right atrial pressure during systole
- Seen as systolic pulsations in the neck
- Often associated with loss of ‘x’ descent
- Confused with carotid pulse if not carefully examined
9. What does the ‘y’ descent in JVP indicate?
- Opening of the tricuspid valve
- Rapid right ventricular filling
- Follows the ‘v’ wave
- Prominent in constrictive pericarditis
- Blunted in tamponade
10. When is the ‘y’ descent prominent?
- Constrictive pericarditis
- Severe right heart failure
- Tricuspid regurgitation (if flow is preserved)
- High-output states
- Absence of pericardial tamponade
11. When is the ‘y’ descent blunted or absent?
- Cardiac tamponade
- Severe tricuspid stenosis
- Pericardial effusion under pressure
- Right atrial mass
- Mechanical obstruction to tricuspid inflow
12. What causes cannon ‘a’ waves in JVP?
- AV dissociation (e.g., complete heart block)
- Atrial contraction against closed tricuspid valve
- Varying intensity with irregular AV timing
- Seen in ventricular tachycardia
- Occasional in junctional rhythm
13. What waveform change is seen in tricuspid regurgitation?
- Giant ‘v’ waves
- Loss of ‘x’ descent
- Rapid y-descent
- Pulsatile neck veins
- Systolic flickering in JVP waveform
14. What waveform abnormalities occur in constrictive pericarditis?
- Prominent ‘x’ and ‘y’ descents
- Rapid y-descent (“Friedrich’s sign”)
- Elevated baseline JVP
- Preserved ‘a’ wave
- Square root sign on pressure tracing
15. What JVP features are typical in cardiac tamponade?
- Elevated JVP
- Prominent ‘x’ descent
- Blunted or absent ‘y’ descent
- Muffled heart sounds and hypotension (Beck’s triad)
- No pulsus paradoxus in JVP waveform
16. How does atrial fibrillation affect the JVP waveform?
- Loss of ‘a’ wave
- Irregular baseline
- Dominant ‘v’ waves
- Variable y-descent
- No atrial contribution to ventricular filling
17. What is the clinical relevance of a steep y-descent?
- Suggests rapid RV filling
- Seen in tricuspid regurgitation
- Typical in constrictive pericarditis
- Helps differentiate from tamponade
- Useful in assessing diastolic function
18. What is a “frog sign” in JVP?
- Bilobed giant ‘a’ waves
- Seen in AVNRT (AV nodal reentrant tachycardia)
- Represents simultaneous atrial and ventricular contraction
- Neck veins bulge with each beat
- Sign of AV dissociation during tachycardia
19. What JVP waveform is seen in complete heart block?
- Regular cannon ‘a’ waves
- AV dissociation pattern
- Independent atrial and ventricular activity
- Variable pulse–JVP relationships
- Often confused with carotid pulse
20. What are Kussmaul’s sign features in JVP?
- Paradoxical rise in JVP on inspiration
- Seen in constrictive pericarditis
- Indicates impaired RV filling
- Absent in tamponade
- Opposite of normal JVP physiology


