Hypothyroidism
Hypothyroidism
Hypothyroidism is likely the most common thyroid disorder encountered in clinical practice
Most common form of primary hypothyroidism in iodine-suffi cient areas of the world is chronic autoimmune (Hashimoto’s) thyroiditis.
Wolff-Chaikoff effect
High doses of exogenous iodides decrease the organifi cation of iodide within the thyroid gland, resulting in a decrease in thyroid hormone synthesis (Wolff-Chaikoff effect).
Amiodarone
It is estimated that a 200-mg dose of amiodarone releases 6 mg/day of iodine
into circulation, compared to the 0.3 mg/day of iodine in the typical
diet in the United States
Lithium carbonate
- Lithium carbonate – medication commonly used to treat bipolar disorder, can significantly impact thyroid function by inhibiting the release of thyroid hormones
- Lithium carbonate – often lead to hypothyroidism (low thyroid hormone levels) and the development of a goiter (enlarged thyroid gland)
Hypothyroidism
What is hypothyroidism?
A condition where the thyroid gland produces insufficient thyroid hormones.
Most common cause of hypothyroidism worldwide?
Iodine deficiency.
Most common autoimmune cause?
Hashimoto’s thyroiditis.
Primary hypothyroidism lab pattern?
High TSH, low free T4.
Classic symptom of hypothyroidism?
Cold intolerance.
What is myxedema?
Non-pitting edema caused by mucopolysaccharide buildup in hypothyroidism.
Which antibody is elevated in Hashimoto’s?
Anti-thyroid peroxidase (anti-TPO) antibody.
Preferred treatment?
Levothyroxine (T4).
Common physical sign in hypothyroidism?
Delayed relaxation of deep tendon reflexes.
Effect on cholesterol?
Increased LDL cholesterol.
Congenital hypothyroidism is called?
Cretinism.
Typical pulse rate?
Bradycardia.
Usual menstrual abnormality?
Menorrhagia (heavy periods).
Effect on skin?
Dry, coarse skin.
Major complication of untreated severe hypothyroidism?
Myxedema coma.
Common drug causing hypothyroidism?
Amiodarone.
Imaging test to assess thyroid size?
Ultrasound thyroid.
How is secondary hypothyroidism characterized?
Low TSH and low T4 due to pituitary/hypothalamic failure.
Effect of hypothyroidism on metabolism?
Decreased basal metabolic rate.
Typical ECG finding?
Low voltage complexes and bradycardia.
| No. | Question | Answer |
|---|---|---|
| 1 | What is hypothyroidism? | Insufficient thyroid hormone production. |
| 2 | Most common cause worldwide? | Iodine deficiency. |
| 3 | Common autoimmune cause? | Hashimoto’s thyroiditis. |
| 4 | Lab pattern in primary hypothyroidism? | High TSH, low free T4. |
| 5 | Classic symptom? | Cold intolerance. |
| 6 | What is myxedema? | Non-pitting edema from mucopolysaccharides. |
| 7 | Elevated antibody in Hashimoto’s? | Anti-thyroid peroxidase (anti-TPO). |
| 8 | Preferred treatment? | Levothyroxine (T4). |
| 9 | Common physical sign? | Delayed deep tendon reflex relaxation. |
| 10 | Effect on cholesterol? | Increased LDL cholesterol. |
| 11 | Congenital hypothyroidism called? | Cretinism. |
| 12 | Typical pulse rate? | Bradycardia. |
| 13 | Menstrual abnormality? | Menorrhagia (heavy bleeding). |
| 14 | Skin changes? | Dry, coarse skin. |
| 15 | Major complication? | Myxedema coma. |
| 16 | Drug causing hypothyroidism? | Amiodarone. |
| 17 | Imaging for thyroid size? | Thyroid ultrasound. |
| 18 | Secondary hypothyroidism labs? | Low TSH and low T4. |
| 19 | Effect on metabolism? | Decreased basal metabolic rate. |
| 20 | Typical ECG finding? | Bradycardia with low voltage complexes. |
| Aspect | Details |
|---|---|
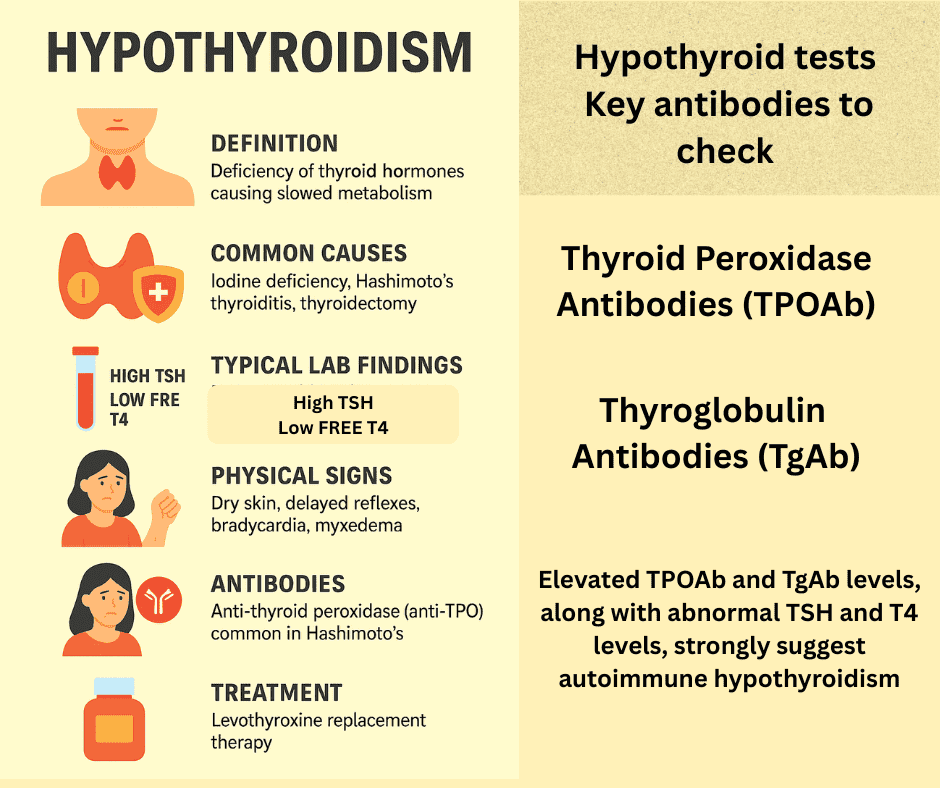
| Definition | Deficiency of thyroid hormones causing slowed metabolism. |
| Common Causes | Iodine deficiency, Hashimoto’s thyroiditis, thyroidectomy. |
| Typical Lab Findings | High TSH, low free T4 (primary hypothyroidism). |
| Common Symptoms | Fatigue, cold intolerance, weight gain, constipation. |
| Physical Signs | Dry skin, delayed reflexes, bradycardia, myxedema. |
| Antibodies | Anti-thyroid peroxidase (anti-TPO) common in Hashimoto’s. |
| Treatment | Levothyroxine replacement therapy. |
| Complications | Myxedema coma, infertility, hypercholesterolemia. |
| Congenital Hypothyroidism | Called cretinism; leads to developmental delay if untreated. |
| Effects on Metabolism | Reduced basal metabolic rate causing fatigue and weight gain. |
Key points:
| Key points: Diagnosis of autoimmune thyroid diseases | |
| • The presence of antibodies is used to confirm the diagnosis of autoimmune thyroid diseases. • Some people will test positive for more than one type of thyroid antibody. • It is possible to test positive for thyroid antibodies without having thyroid disease. • It is rarely useful to repeat measurements of TPOAb as their level does not influence the treatment given. • Thyroid antibodies often remain in the body even after the thyroid disorder has been successfully treated. • The presence of antibodies in a person with subclinical (or borderline) thyroid disease can indicate a person may go on to develop full-blown thyroid disease in the future. |


