Echocardiography findings in Hypertrophic Cardiomyopathy
Echocardiography findings in hypertrophic cardiomyopathy
1. What is the hallmark echocardiographic feature of hypertrophic cardiomyopathy?
A. Dilated left ventricle with reduced EF
B. Right ventricular hypertrophy
C. Asymmetric septal hypertrophy
D. Apical ballooning
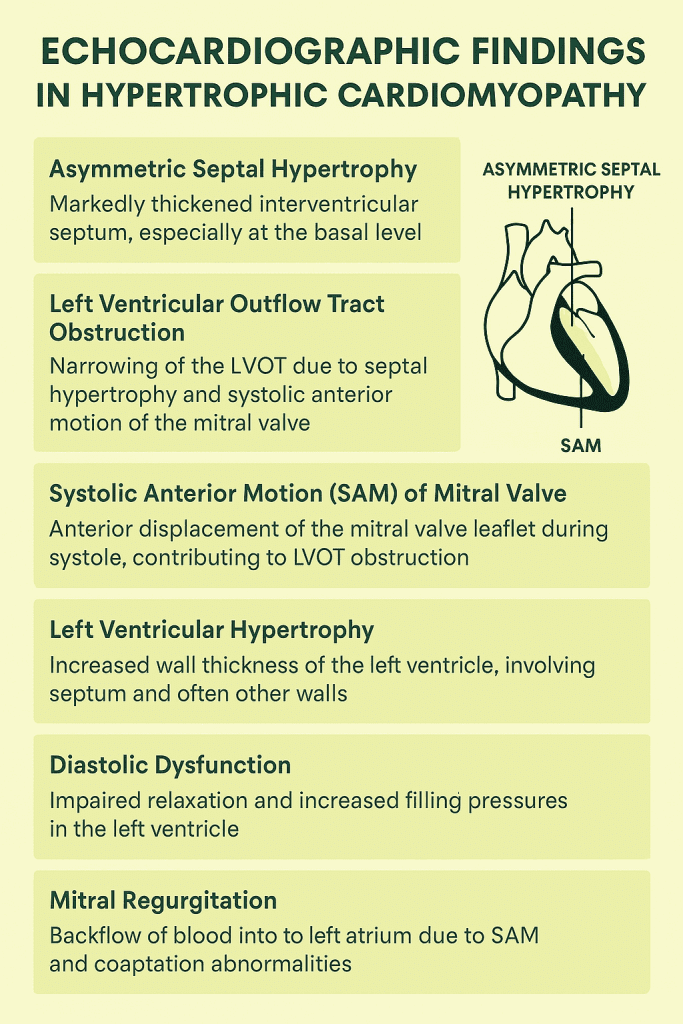
Explanation: The most common and characteristic finding in HCM is asymmetric septal hypertrophy, especially involving the basal interventricular septum.
2. Systolic anterior motion (SAM) of the mitral valve is best associated with:
A. Left ventricular outflow tract (LVOT) obstruction
B. Mitral valve prolapse
C. Aortic regurgitation
D. Diastolic dysfunction
Explanation: SAM causes dynamic obstruction in the LVOT during systole, a classic finding in obstructive HCM.
3. Which Doppler finding is typically seen in obstructive HCM?
A. Continuous flow in LVOT
B. Late-peaking systolic jet in LVOT
C. Diastolic forward flow in aorta
D. Mid-systolic aortic regurgitation
Explanation: A classic Doppler feature in obstructive HCM is a late-peaking systolic jet through the LVOT, indicating dynamic obstruction.
4. What is the typical mitral valve motion seen in HCM?
A. Restrictive opening
B. Systolic anterior motion
C. Diastolic prolapse
D. Holosystolic prolapse
Explanation: Systolic anterior motion (SAM) of the mitral valve is a hallmark feature in obstructive forms of HCM.
5. Which of the following is the best imaging modality to assess myocardial fibrosis in HCM?
A. Contrast-enhanced echocardiography
B. Stress echocardiography
C. Cardiac MRI with late gadolinium enhancement
D. CT coronary angiography
Explanation: Cardiac MRI with late gadolinium enhancement is the gold standard for assessing myocardial fibrosis in HCM.
6. Apical variant of HCM shows hypertrophy predominantly in:
A. Basal interventricular septum
B. Posterior wall
C. Left ventricular apex
D. Right ventricular free wall
Explanation: In apical HCM, hypertrophy is localized to the apex of the left ventricle, and is best seen on apical 4-chamber views or MRI.
7. Which echocardiographic view best shows SAM of the mitral valve?
A. Apical four-chamber
B. Parasternal long axis
C. Subcostal view
D. Suprasternal view
Explanation: SAM is most clearly visualized in the parasternal long axis view, which aligns well with the mitral valve and LVOT.
8. Which of the following is commonly associated with HCM in echocardiography?
A. Thin interventricular septum
B. Mitral regurgitation due to SAM
C. Right atrial enlargement
D. Pericardial effusion
Explanation: SAM of the mitral valve in HCM leads to mitral regurgitation, a common echocardiographic finding.
9. Which measurement best quantifies LVOT gradient in HCM?
A. LA volume index
B. Continuous wave Doppler peak velocity
C. LV end-diastolic diameter
D. Wall motion index
Explanation: Continuous wave Doppler is used to assess peak velocity across the LVOT, from which pressure gradient is calculated.
10. What type of hypertrophy is most typical in classic HCM?
A. Concentric hypertrophy
B. Asymmetric septal hypertrophy
C. Apical hypertrophy
D. Right ventricular hypertrophy
Explanation: Asymmetric septal hypertrophy, often with a septal-to-posterior wall thickness ratio >1.3:1, is the hallmark of classic HCM.
11. What does a “speckled” myocardial texture on echo suggest in HCM?
A. Fatty infiltration
B. Myocardial disarray and fibrosis
C. Amyloidosis
D. Hemochromatosis
Explanation: The speckled or granular appearance of the myocardium in HCM may indicate myocardial fibrosis and disarray.
12. What feature helps differentiate athlete’s heart from HCM on echo?
A. Increased LV wall thickness >15 mm
B. LVOT gradient
C. Normal diastolic function and cavity size
D. Systolic anterior motion
Explanation: Athlete’s heart typically has normal or enhanced diastolic function and increased cavity size, unlike HCM.
13. LVOT obstruction in HCM is often provoked by:
A. Beta-blockers
B. Valsalva maneuver
C. High preload
D. Leg elevation
Explanation: Maneuvers like Valsalva reduce preload and enhance the LVOT gradient, provoking obstruction.
14. What is a risk marker for sudden cardiac death in HCM?
A. Apical HCM
B. Max wall thickness >30 mm
C. Diastolic dysfunction
D. Age >65 years
Explanation: Maximal wall thickness >30 mm is a strong risk factor for sudden cardiac death in HCM patients.
15. Which echocardiographic parameter suggests diastolic dysfunction in HCM?
A. Increased E/A ratio
B. Elevated E/e’ ratio
C. Decreased LA size
D. Increased deceleration time
Explanation: An elevated E/e’ ratio suggests increased LV filling pressures and is indicative of diastolic dysfunction.
16. What echocardiographic feature helps identify apical HCM?
A. Basal wall thickening
B. Systolic anterior motion
C. Spade-like configuration of LV cavity
D. LVOT obstruction
Explanation: Apical HCM shows a spade-like configuration of the LV cavity on contrast echo or MRI due to isolated apical thickening.
17. In HCM, which of the following indicates severe outflow obstruction?
A. LVOT gradient <30 mmHg
B. LVOT gradient >50 mmHg
C. Reduced mitral inflow velocity
D. Decreased E/e’ ratio
Explanation: A resting or provoked LVOT gradient >50 mmHg is considered significant and may be an indication for intervention.
18. What is the role of contrast echocardiography in HCM?
A. Rule out pericardial effusion
B. Define LV cavity and apex in apical HCM
C. Visualize coronary arteries
D. Diagnose ASD
Explanation: Contrast echocardiography enhances endocardial border definition, aiding in identification of apical hypertrophy in HCM.
19. What abnormal motion is characteristic of mitral valve in HCM?
A. Posterior leaflet prolapse
B. Systolic anterior motion (SAM)
C. Late systolic bowing
D. Valve tethering
Explanation: SAM of the mitral valve is a hallmark feature of HCM and contributes to LVOT obstruction and mitral regurgitation.
20. Which modality is most useful when echo windows are suboptimal in HCM?
A. Chest X-ray
B. Cardiac MRI
C. CT Angiography
D. PET scan
Explanation: Cardiac MRI provides detailed myocardial structure, detects fibrosis, and is valuable when echo images are suboptimal.
Echocardiography findings in Hypertrophic Cardiomyopathy
🧠 Short-Answer Questions (5 points each)
- List three key echocardiographic features of hypertrophic cardiomyopathy.
- What is systolic anterior motion (SAM) of the mitral valve and its clinical significance?
- How can echocardiography differentiate between obstructive and non-obstructive HCM?
- Describe the appearance and significance of a spade-like LV cavity on imaging.
- What role does contrast echocardiography play in diagnosing apical HCM?
- Explain the utility of Doppler echocardiography in assessing LVOT gradient.
- How does mitral regurgitation occur in hypertrophic cardiomyopathy?
- What is the E/e’ ratio and how is it used in HCM evaluation?
- Which echocardiographic findings may indicate poor prognosis in HCM?
- When is cardiac MRI preferred over echocardiography in HCM patients?
Echocardiography findings in Hypertrophic Cardiomyopathy
🧠 Short-Answer Questions (5 points each)
-
List three key echocardiographic features of hypertrophic cardiomyopathy.
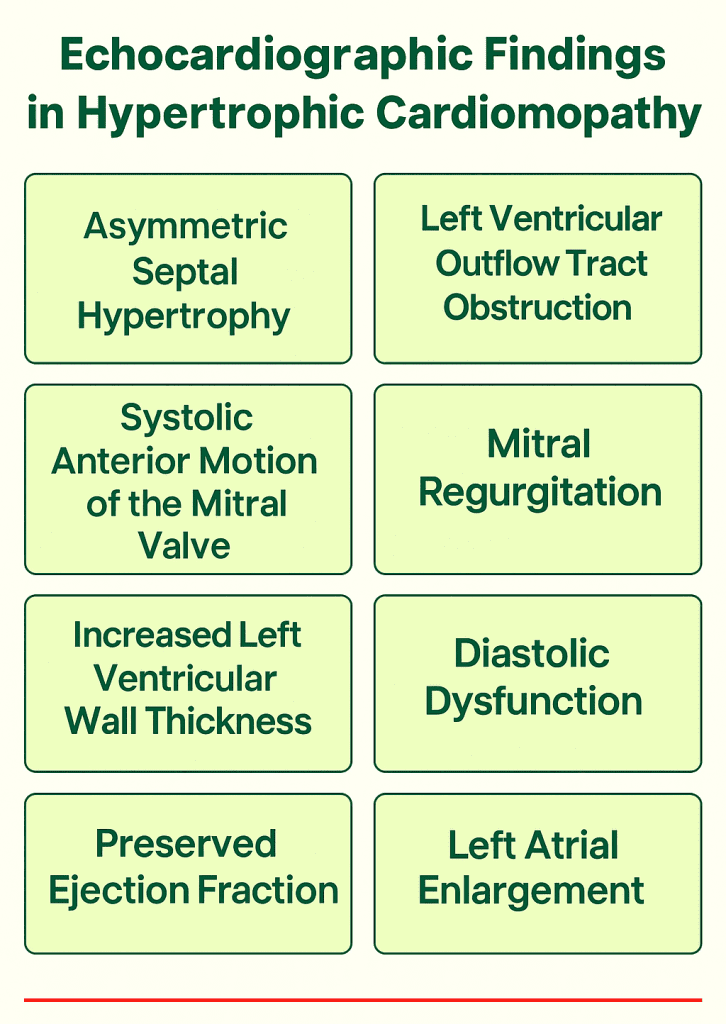
1. Asymmetric septal hypertrophy is the hallmark finding.
2. Systolic anterior motion (SAM) of the mitral valve is commonly observed.
3. LVOT gradient and mitral regurgitation are often detected using Doppler.
4. These findings help identify obstructive vs non-obstructive forms.
5. Essential for diagnosis and management decisions. -
What is systolic anterior motion (SAM) of the mitral valve and its clinical significance?
1. SAM is anterior motion of the mitral valve during systole.
2. It moves toward the interventricular septum, obstructing LVOT.
3. This contributes to dynamic LVOT obstruction.
4. SAM also leads to posteriorly directed mitral regurgitation.
5. Identifying SAM is key to diagnosing obstructive HCM. -
How can echocardiography differentiate between obstructive and non-obstructive HCM?
1. Doppler echocardiography measures the LVOT gradient.
2. Presence of SAM confirms obstruction.
3. Provocative maneuvers can reveal latent obstruction.
4. Non-obstructive HCM lacks significant gradients.
5. Structural imaging must be combined with Doppler assessment. -
Describe the appearance and significance of a spade-like LV cavity on imaging.
1. Seen in apical HCM as a spade-shaped left ventricle.
2. Caused by isolated hypertrophy of the LV apex.
3. Often best seen with contrast echo or MRI.
4. May be associated with deep T-wave inversions on ECG.
5. Prognosis is generally better in apical variants. -
What role does contrast echocardiography play in diagnosing apical HCM?
1. Enhances endocardial border visualization.
2. Especially useful for identifying apical hypertrophy.
3. Helps confirm diagnosis when images are suboptimal.
4. Clarifies regional wall thickness and cavity shape.
5. Complements standard transthoracic echocardiography. -
Explain the utility of Doppler echocardiography in assessing LVOT gradient.
1. Doppler measures peak LVOT velocity during systole.
2. The Bernoulli equation converts velocity to pressure gradient.
3. Gradients >30 mmHg are clinically significant.
4. Helps classify obstructive vs non-obstructive HCM.
5. Stress or Valsalva may reveal latent obstruction. -
How does mitral regurgitation occur in hypertrophic cardiomyopathy?
1. SAM leads to malcoaptation of mitral valve leaflets.
2. Results in posteriorly directed mitral regurgitation jet.
3. Regurgitation severity varies with obstruction degree.
4. Doppler evaluates MR jet area and direction.
5. Treating obstruction often improves regurgitation. -
What is the E/e’ ratio and how is it used in HCM evaluation?
1. E/e’ ratio estimates left ventricular filling pressure.
2. E is mitral inflow velocity; e’ is annular tissue velocity.
3. Elevated E/e’ suggests diastolic dysfunction.
4. Common in HCM due to stiff myocardium.
5. Helps assess symptoms and guide therapy. -
Which echocardiographic findings may indicate poor prognosis in HCM?
1. Massive LV wall thickness >30 mm.
2. Presence of apical aneurysm or mid-cavity obstruction.
3. Reduced systolic function, though rare, worsens outcomes.
4. Large left atrium and severe MR are poor prognostic signs.
5. Risk stratification is enhanced with MRI findings. -
When is cardiac MRI preferred over echocardiography in HCM patients?
1. Used when echo images are suboptimal.
2. Defines apical and atypical hypertrophy more clearly.
3. Detects myocardial fibrosis with late gadolinium enhancement.
4. Important in surgical or ICD planning.
5. Complements echo for comprehensive evaluation.
📊 20-Point Summary Table: Echocardiography in Hypertrophic Cardiomyopathy
| Feature | Details |
|---|---|
| 1. Septal Hypertrophy | Asymmetric septal thickening >15 mm, hallmark of HCM |
| 2. SAM of Mitral Valve | Anterior motion during systole contributes to LVOT obstruction |
| 3. LVOT Gradient | Peak gradient >30 mmHg is clinically significant |
| 4. Mitral Regurgitation | Often posteriorly directed, secondary to SAM |
| 5. Diastolic Dysfunction | Stiff LV with impaired relaxation; assessed by E/e’ ratio |
| 6. Apical HCM | Spade-shaped cavity; best seen with contrast or MRI |
| 7. Left Atrial Enlargement | Reflects chronic diastolic dysfunction or MR |
| 8. Mid-Cavity Obstruction | May occur with systolic cavity obliteration |
| 9. Apical Aneurysm | Thin, dyskinetic apex; seen in advanced apical HCM |
| 10. Doppler Assessment | Used to quantify gradients and regurgitation |
| 11. Valsalva Maneuver | Helps reveal latent obstruction in borderline cases |
| 12. Provocative Testing | Exercise/stress echo for symptomatic evaluation |
| 13. Ejection Fraction | Often normal or supranormal; systolic dysfunction rare |
| 14. Contrast Echocardiography | Improves LV border definition in apical HCM |
| 15. Tissue Doppler Imaging | e’ velocity aids in assessing diastolic function |
| 16. LA Strain Imaging | Emerging marker for diastolic dysfunction |
| 17. 3D Echocardiography | Useful in mitral valve assessment and volume quantification |
| 18. RV Involvement | Rare, but can occur with biventricular hypertrophy |
| 19. Risk Stratification | Echo aids in predicting sudden cardiac death risk |
| 20. MRI Integration | Adds detail on fibrosis and scar burden, complements echo |
Genetics in Hypertrophic Cardiomyopathy (HCM)
Genetics in Hypertrophic Cardiomyopathy (HCM) 1. What is the most common mode of inheritance in Hypertrophic Cardiomyopathy? A. Autosomal dominant B. Autosomal recessive C. X-linked recessive D. Mitochondrial inheritance 💬 Explanation: HCM is typically inherited in an autosomal dominant fashion, meaning one copy of the mutated gene is sufficient to cause disease. 2. Which gene is most commonly mutated in HCM? A. MYBPC3 B. ACTN2 C. LMNA D. DMD 💬 Explanation: MYBPC3 is the most commonly mutated gene in HCM, especially in Western populations. 3. Mutations in which of the following genes are associated with early-onset and more severe HCM?...


