Current Status of Pharmaco-Invasive Therapy in STEMI
Current Status of Pharmaco-Invasive Therapy in STEMI
1. What is the goal of pharmaco-invasive therapy in STEMI?
A. Delay revascularization to avoid complications
B. Replace PCI completely with thrombolytics
C. Initiate fibrinolysis followed by timely PCI
D. Use anticoagulation only for symptom control
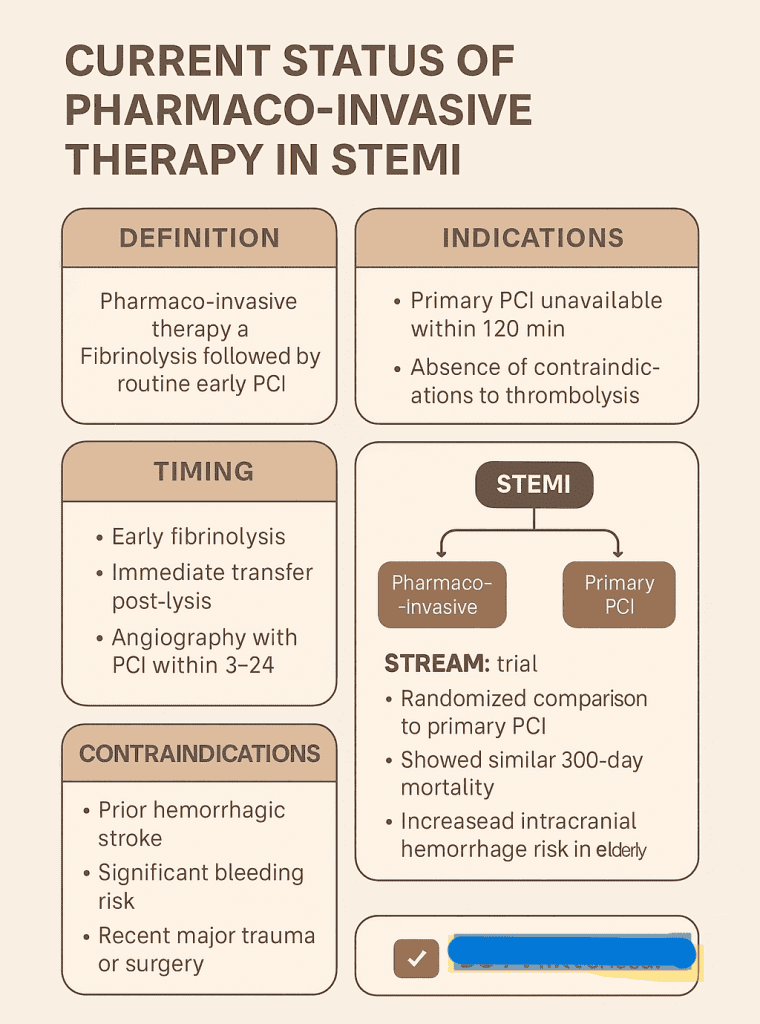
💬 Explanation: Pharmaco-invasive therapy uses early fibrinolysis when PCI is unavailable, followed by PCI within 3–24 hours.
2. The recommended time window for PCI after fibrinolysis in pharmaco-invasive strategy is:
A. 48–72 hours
B. 3–24 hours
C. After 7 days
D. Immediately after thrombolysis
💬 Explanation: PCI is ideally performed within 3–24 hours after thrombolysis in pharmaco-invasive strategy.
3. Pharmaco-invasive strategy is especially useful in:
A. All stable angina patients
B. Patients within 12 hours with ongoing symptoms near PCI center
C. STEMI patients where PCI cannot be done within 120 minutes
D. NSTEMI patients with delayed presentation
💬 Explanation: It’s best used when timely primary PCI is not possible due to logistics or location.
4. Which fibrinolytic agent is most commonly used in pharmaco-invasive therapy?
A. Streptokinase
B. Tenecteplase
C. Urokinase
D. Alteplase bolus
💬 Explanation: Tenecteplase is preferred due to ease of administration (single bolus) and efficacy.
5. STREAM trial evaluated:
A. Pharmaco-invasive therapy vs primary PCI
B. Bivalirudin vs heparin
C. DAPT in NSTEMI
D. CABG vs PCI in stable angina
💬 Explanation: The STREAM trial showed non-inferiority of a pharmaco-invasive approach to primary PCI.
6. What is the main limitation of pharmaco-invasive therapy?
A. No mortality benefit
B. Risk of bleeding with fibrinolysis
C. Delay in thrombolysis
D. Infeasibility in rural areas
💬 Explanation: Fibrinolysis carries higher bleeding risk, especially in elderly patients.
7. Pharmaco-invasive therapy is preferred over primary PCI when:
A. PCI is available within 60 minutes
B. PCI cannot be done within 120 minutes
C. Patient has prior CABG
D. STEMI > 24 hours old
💬 Explanation: It is a bridge strategy when PCI delays are expected to exceed 120 minutes.
8. After successful fibrinolysis, which of the following is next in pharmaco-invasive strategy?
A. Immediate transfer for CABG
B. Observation only
C. Scheduled PCI within 3–24 hours
D. Repeat thrombolysis
💬 Explanation: Early PCI (3–24 hrs) improves patency and outcomes after thrombolysis.
9. STREAM trial protocol excluded patients:
A. With inferior MI
B. Older than 75 years (initially)
C. Presenting within 3 hours
D. Already on DAPT
💬 Explanation: Due to bleeding risk, initial protocol excluded patients >75 years, later amended with half-dose tenecteplase.
10. Compared to primary PCI, pharmaco-invasive therapy shows:
A. Comparable mortality in low-resource settings
B. Higher mortality in all settings
C. Always worse outcomes
D. No benefit in reducing infarct size
💬 Explanation: It provides a viable alternative to primary PCI where infrastructure limits rapid access.
11. Which guideline supports pharmaco‑invasive strategy when PCI delay >120 min?
A. ESC STEMI Guidelines
B. US hypertension guidelines
C. Dyslipidemia guidelines
D. Heart failure guidelines
💬 Explanation: ESC (and ACC/AHA) STEMI guidelines recommend pharmaco‑invasive therapy if primary PCI cannot be achieved within 120 minutes.
12. Which patient should receive half‑dose tenecteplase in STREAM protocol?
A. Age < 50
B. Age > 75 years
C. Female gender
D. Diabetes mellitus
💬 Explanation: Patients > 75 were given half‑dose tenecteplase in STREAM to reduce bleeding risk.
13. After thrombolysis, when is rescue PCI indicated?
A. At 48 hours despite reperfusion
B. If fibrinolysis fails (ongoing pain, STEMI persistent)
C. Only if angiography shows stenosis
D. Never within the first week
💬 Explanation: Rescue PCI is required if reperfusion fails: persistent chest pain or <50% ST‑segment resolution.
14. STREAM trial showed which primary outcome result?
A. Non‐inferiority in 30‑day mortality
B. Higher mortality vs PCI
C. Major hemorrhage benefit
D. Superior long‑term survival
💬 Explanation: STREAM demonstrated non‑inferiority of pharmaco‑invasive therapy compared to primary PCI for 30‑day mortality.
15. Which is a key contraindication to pharmaco‑invasive fibrinolysis?
A. History of hemorrhagic stroke
B. Controlled hypertension
C. Minor head trauma months ago
D. Age > 85 if weighed accurately
💬 Explanation: Hemorrhagic stroke is an absolute contraindication to fibrinolysis.
16. What is the recommended antithrombotic regimen post‑fibrinolysis before PCI?
A. Warfarin only
B. Aspirin + P2Y₁₂ inhibitor + heparin or enoxaparin
C. Dual therapy not needed
D. Direct thrombin inhibitor only
💬 Explanation: Standard care: aspirin, P2Y₁₂ inhibitor plus anticoagulation until PCI.
17. What complication was slightly increased in STREAM’s thrombolysis arm?
A. Intracranial hemorrhage (in older patients)
B. Acute kidney injury
C. Stroke from thrombus
D. Contrast‑induced nephropathy
💬 Explanation: STREAM showed a slightly higher rate of intracranial hemorrhage in patients > 75 treated with standard dose tenecteplase.
18. How soon should transfer to PCI centre occur post‑thrombolysis?
A. Within 3–24 hours
B. After 48 hours
C. Only if symptoms recur
D. After 7 days
💬 Explanation: Early transfer improves patency, reduces reinfarction and complications.
19. What is a benefit of pharmaco‑invasive strategy in rural settings?
A. No need for DAPT
B. Enables early reperfusion despite PCI delays
C. Eliminates need for hospital transfer
D. Reduces need for anticoagulation
💬 Explanation: It allows timely reperfusion where primary PCI is delayed or inaccessible.
20. What should hospitals implement to support pharmaco‑invasive care pathways?
A. Only primary PCI teams
B. Delayed transfer networks
C. Pre‑hospital thrombolysis + transfer protocol
D. No network coordination needed
💬 Explanation: Coordinated pre-hospital fibrinolysis and transfer protocols are essential for effective pharmaco‑invasive care.
Current Status of Pharmaco-Invasive Therapy in STEMI
| # | Current Status of Pharmaco-Invasive Therapy in STEMI |
|---|---|
| 1 | Pharmaco-invasive therapy involves fibrinolysis followed by early PCI. |
| 2 | Recommended when primary PCI cannot be performed within 120 minutes. |
| 3 | Tenecteplase is the most commonly used fibrinolytic in this setting. |
| 4 | Older adults (>75) require half-dose tenecteplase to reduce bleeding risk. |
| 5 | STREAM trial supports the efficacy and safety of this strategy. |
| 6 | 30-day mortality is non-inferior to primary PCI when promptly followed by PCI. |
| 7 | Rescue PCI is needed if reperfusion fails (persistent ST elevation or pain). |
| 8 | Routine angiography and PCI should be performed within 3–24 hours post-lysis. |
| 9 | Antiplatelets and anticoagulants should be continued until PCI is done. |
| 10 | Avoid fibrinolysis in patients with prior hemorrhagic stroke or bleeding risks. |
| 11 | Intracranial hemorrhage is a known complication, especially in the elderly. |
| 12 | Dual antiplatelet therapy is mandatory before and after PCI. |
| 13 | Early administration of fibrinolytics improves outcomes in remote settings. |
| 14 | This strategy bridges delays in primary PCI in rural/underserved regions. |
| 15 | Streamlined transfer to PCI centers is crucial for success. |
| 16 | Should not be used in non-STEMI or unclear STEMI diagnosis. |
| 17 | Pre-hospital thrombolysis systems can shorten reperfusion time significantly. |
| 18 | Health systems should develop pharmaco-invasive protocols and training. |
| 19 | Follow-up and risk stratification after PCI remains vital. |
| 20 | Overall, a pharmaco-invasive approach is evidence-based and practical in real-world delays. |
-
Define pharmaco-invasive strategy in STEMI.
• Combines thrombolysis and early PCI
• Used when primary PCI is delayed >120 mins
• Involves early fibrinolytic administration
• Followed by angiography within 3–24 hrs
• Goal: timely reperfusion when PCI unavailable -
List advantages of pharmaco-invasive therapy.
• Early reperfusion in remote areas
• Reduces total ischemic time
• Comparable mortality to primary PCI
• More feasible than timely primary PCI
• Better than thrombolysis alone -
What did the STREAM trial show?
• Compared pharmaco-invasive vs primary PCI
• Showed non-inferior 30-day mortality
• Increased early ICH risk in elderly
• Supported early PCI post-fibrinolysis
• Validated pharmaco-invasive model -
When is rescue PCI indicated?
• Ongoing chest pain after thrombolysis
• ST elevation not resolved by >50% in 90 mins
• Hemodynamic instability
• Development of arrhythmias
• High-risk features post-lysis -
Name common agents used for lysis.
• Tenecteplase
• Alteplase
• Reteplase
• Streptokinase (less favored)
• Use adjusted for age/weight -
Contraindications to fibrinolysis?
• Prior hemorrhagic stroke
• Recent surgery or trauma
• Active internal bleeding
• Known intracranial lesion
• Severe uncontrolled hypertension -
Outline post-lysis PCI timing guidelines.
• Rescue PCI: immediate if failed lysis
• Routine PCI: 3–24 hours post-lysis
• Urgent PCI if unstable
• Delay >24 hrs only if stable/low-risk
• Avoid early cath <3 hrs unless rescue needed -
What’s the role of antiplatelets in this strategy?
• Aspirin is mandatory
• Clopidogrel loading after lysis
• Continue DAPT till PCI
• Use heparin until cath
• Adjust P2Y12 based on bleeding risk -
Why is pharmaco-invasive strategy ideal in LMICs?
• Limited cath lab availability
• Long transport times
• Easier access to fibrinolysis
• Cost-effective compared to PPCI
• Enables structured transfer to PCI centers -
Major limitations of pharmaco-invasive therapy?
• Bleeding risk
• Risk of failed thrombolysis
• Requires structured referral system
• Not suitable in ambiguous STEMI
• Less effective in late presenters