Myocardial Infarction – troponin levels in myocardial infarction
Contents
- 1 Troponin levels in myocardial infarction
- 2 1. Which of the following troponin isoforms is considered the most cardiac-specific biomarker for diagnosing myocardial infarction?
- 3 2. What is the key advantage of high-sensitivity troponin assays (hs-cTn) over conventional assays in diagnosing acute myocardial infarction?
- 4 3. Which of the following statements best describes the kinetics of troponin I following an acute myocardial infarction?
- 5 4. In the context of chronic kidney disease (CKD), elevated troponin levels are best interpreted by:
- 6 5. Which of the following is a limitation of high-sensitivity troponin assays in clinical practice?
- 7 6. According to the Fourth Universal Definition of Myocardial Infarction, a diagnosis of type 1 MI requires:
- 8 7. In the ESC 0/1-hour algorithm for rule-out of MI, what is the role of high-sensitivity troponin measurements?
- 9 8. Which post-translational modification of cardiac troponin I is associated with increased degradation in ischemic myocardium?
- 10 Troponin levels in myocardial infarction
- 11 Biological and Biochemical Aspects
- 12 Clinical and Diagnostic Importance
- 13 Interpretation and Use in Medicine
- 14 Troponin levels in myocardial infarction
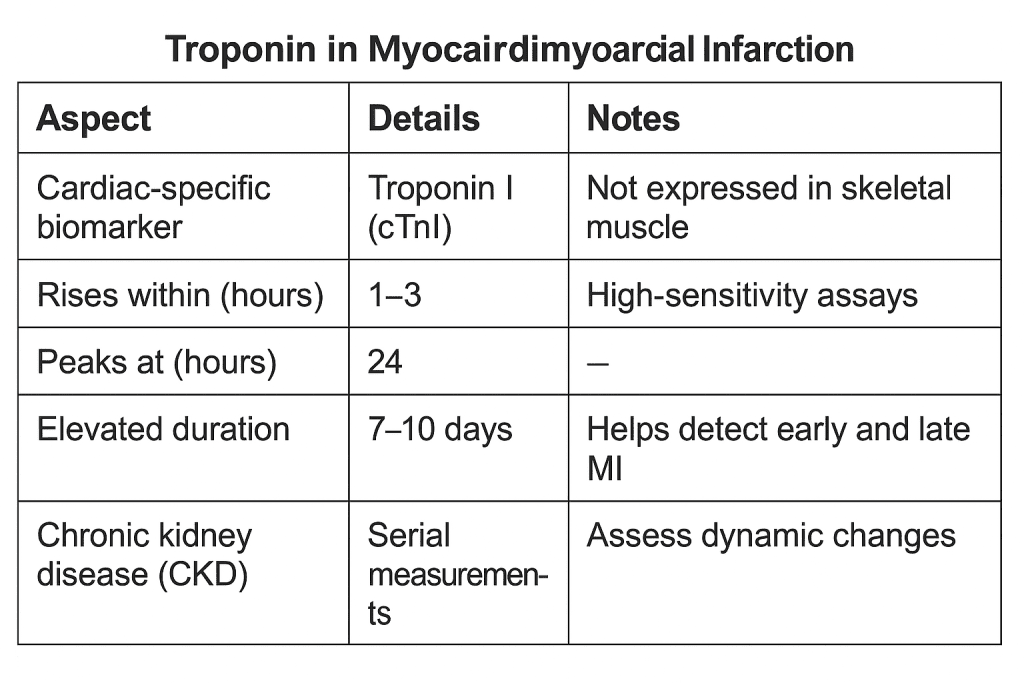
Troponin levels in myocardial infarction
1. Which of the following troponin isoforms is considered the most cardiac-specific biomarker for diagnosing myocardial infarction?
A. Troponin C
B. Troponin T (cTnT)
C. Troponin I (cTnI)
D. Troponin T and I equally
Correct Answer: C
Explanation: Troponin I (cTnI) is highly specific to cardiac muscle and not expressed in skeletal muscle, making it a more specific marker for myocardial injury compared to cTnT, which may be expressed in skeletal muscle in certain pathologies.
2. What is the key advantage of high-sensitivity troponin assays (hs-cTn) over conventional assays in diagnosing acute myocardial infarction?
A. Better specificity for skeletal muscle injury
B. Detection of myocardial necrosis earlier
C. No false positives in renal failure
D. Cost-effectiveness in emergency settings
Correct Answer: B
Explanation: High-sensitivity troponin assays can detect very low levels of troponin, allowing earlier diagnosis of myocardial infarction (as early as 1–2 hours from symptom onset).
3. Which of the following statements best describes the kinetics of troponin I following an acute myocardial infarction?
A. Rises within 30 minutes, peaks at 6 hours, normalizes in 12 hours
B. Rises within 1–3 hours, peaks at 24 hours, remains elevated for 7–10 days
C. Rises within 6 hours, peaks at 72 hours, remains elevated for 1 month
D. Rises only after 24 hours, peaks at 48 hours, remains elevated for 5 days
Correct Answer: B
Explanation: Troponin I begins to rise within 1–3 hours, peaks at 24 hours, and remains elevated for 7–10 days, which helps in detecting both early and late presentations of MI.
4. In the context of chronic kidney disease (CKD), elevated troponin levels are best interpreted by:
A. Considering troponin as invalid due to renal clearance issues
B. Using serial measurements to assess dynamic changes
C. Comparing with creatinine kinase-MB levels
D. Relying solely on ECG and symptoms
Correct Answer: B
Explanation: In CKD, baseline troponin levels may be elevated chronically. Serial measurements showing a rise and/or fall pattern are essential to diagnose acute MI in these patients.
5. Which of the following is a limitation of high-sensitivity troponin assays in clinical practice?
A. Cannot detect microinfarcts
B. Lead to higher false negatives
C. Increase detection of type 2 MIs and non-ischemic causes of troponin elevation
D. Not useful for early discharge protocols
Correct Answer: C
Explanation: High-sensitivity assays may detect low-level troponin elevations due to other causes like sepsis, tachyarrhythmias, or heart failure (type 2 MI), leading to diagnostic challenges in distinguishing true type 1 MI.
6. According to the Fourth Universal Definition of Myocardial Infarction, a diagnosis of type 1 MI requires:
A. Any elevation in troponin
B. Troponin rise and/or fall with at least one value above the 99th percentile URL plus clinical evidence of myocardial ischemia
C. Troponin elevation plus BNP >500
D. Troponin elevation plus CRP >10 mg/L
Correct Answer: B
Explanation: The definition of MI includes a rise and/or fall in troponin values with at least one value above the 99th percentile upper reference limit, along with clinical evidence of ischemia (symptoms, ECG changes, imaging, etc.).
7. In the ESC 0/1-hour algorithm for rule-out of MI, what is the role of high-sensitivity troponin measurements?
A. To confirm MI based on static levels
B. To determine long-term mortality
C. To rapidly rule in or rule out MI based on troponin changes within 1 hour
D. To evaluate chronic cardiac disease
Correct Answer: C
Explanation: The ESC 0/1-hour algorithm uses serial hs-cTn measurements at presentation and 1 hour later to quickly rule in or rule out acute MI, aiding early decision-making in emergency settings.
8. Which post-translational modification of cardiac troponin I is associated with increased degradation in ischemic myocardium?
A. Methylation
B. Phosphorylation
C. Ubiquitination
D. Glycosylation
Correct Answer: B
Explanation: Phosphorylation of cardiac troponin I by kinases (e.g., PKA, PKC) in response to ischemia leads to changes in conformation, enhancing degradation and release into circulation.
Troponin levels in myocardial infarction
Biological and Biochemical Aspects
- Troponin is a protein complex found in skeletal and cardiac muscle that regulates muscle contraction by controlling the interaction between actin and myosin.
- It consists of three subunits:
- Troponin C (TnC): Binds calcium ions.
- Troponin I (TnI): Inhibits actomyosin ATPase.
- Troponin T (TnT): Binds the troponin complex to tropomyosin.
- Troponin is specific to muscle tissue, with cardiac-specific isoforms (cTnI and cTnT) that differ from skeletal forms, making them useful biomarkers for cardiac injury.
- Calcium binding to TnC causes a conformational change that shifts tropomyosin away from actin’s myosin-binding sites, initiating contraction.
- Cardiac troponins are encoded by distinct genes from those encoding skeletal muscle isoforms, which allows for high specificity in clinical testing.
Clinical and Diagnostic Importance
- Cardiac troponins (cTnI and cTnT) are gold-standard biomarkers for diagnosing myocardial infarction (MI).
- They are released into the bloodstream following myocardial injury, typically starting 3–6 hours after injury and remaining elevated for up to 14 days.
- High-sensitivity troponin assays (hs-cTn) allow for earlier and more accurate detection of myocardial injury.
- Troponin levels correlate with the extent of myocardial damage, making them useful for risk stratification and prognosis.
- Troponin elevation is not exclusive to MI – it can occur in heart failure, myocarditis, pulmonary embolism, renal failure, and sepsis.
Interpretation and Use in Medicine
- Serial measurements of troponin (typically over 3–6 hours) are essential to confirm dynamic changes consistent with acute myocardial infarction.
- The 99th percentile of a reference population is used as the diagnostic cutoff value for elevated troponin levels.
- Troponin testing is integrated into the Universal Definition of Myocardial Infarction, especially in type 1 MI (due to plaque rupture) and type 2 MI (due to oxygen supply-demand mismatch).
- Troponin assays vary between labs, so clinicians must be familiar with the specific reference values used in their institutions.
- Elevated troponin has prognostic significance, even in non-coronary conditions; it is associated with worse outcomes.
Troponin levels in myocardial infarction
| 1 | Troponin is a protein complex found in skeletal and cardiac muscle that regulates contraction. |
| 2 | It consists of three subunits: TnC (calcium-binding), TnI (inhibitory), and TnT (tropomyosin-binding). |
| 3 | Troponin is specific to muscle tissue, with cardiac-specific isoforms (cTnI and cTnT). |
| 4 | Calcium binding to TnC initiates a conformational change allowing muscle contraction. |
| 5 | Cardiac troponins are encoded by different genes than skeletal forms, ensuring diagnostic specificity. |
| 6 | Cardiac troponins (cTnI, cTnT) are the gold standard biomarkers for myocardial infarction diagnosis. |
| 7 | Troponins are released into the bloodstream 3–6 hours post-myocardial injury, staying elevated for days. |
| 8 | High-sensitivity troponin assays (hs-cTn) improve early detection of myocardial injury. |
| 9 | Troponin levels correlate with the extent of myocardial damage. |
| 10 | Elevated troponin is not exclusive to MI; it can occur in other conditions (e.g., renal failure, sepsis). |
| 11 | Serial measurements are crucial to observe dynamic changes and confirm MI. |
| 12 | The 99th percentile of a reference population is used as the diagnostic cutoff. |
| 13 | Troponin testing is central to the Universal Definition of Myocardial Infarction. |
| 14 | Different assays may yield different results; reference values vary by institution. |
| 15 | Troponin elevation has prognostic value in both cardiac and non-cardiac conditions. |
| 17 | Chronic low-level troponin elevation may indicate subclinical cardiovascular disease. |
| 18 | Athletes may show temporary troponin elevation after intense exercise. |